Reach out to our compassionate team of experts for help with your journey to recovery. We’re here to support you every step of the way.
If you’re concerned about a friend or family member’s well-being, we’re here to guide them on their path to recovery. Let us be your partner in their healing journey.
Ensure you have the support you need by verifying your insurance coverage. We’ll assist you in understanding your options and getting the treatment you deserve.
While some recovery centers take an institutional approach to drug rehab, Crest View Recovery Center in Asheville, NC prefers to provide our patients with a realistic recovery environment and allow room for true growth and discovery.

Experience personalized support for alcohol recovery at Crest View Recovery Center, where we prioritize genuine growth in a realistic environment.

Find a caring path to overcome opiate addiction at Crest View Recovery Center, where we focus on real-life experiences for true growth and recovery.

Choose Crest View Recovery Center for integrated care in dual diagnosis. Our approach addresses mental health and substance use, fostering genuine recovery.
Located in the beautiful Western mountains of Asheville, North Carolina, Crest View Recovery Center is a safe haven for life-changing addiction recovery. Take a tour of our facilities and see why Crestview is the perfect place to start a new, substance-free life.
Andrew’s life was spinning out of control, he knew it was time to make a change. Watch our video to hear about Andrew’s Crest View Recovery Center experience.
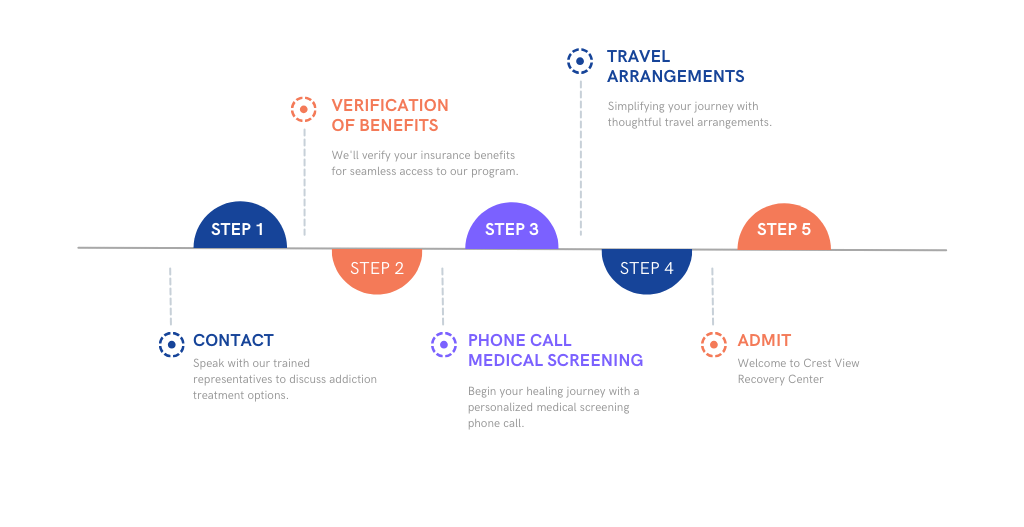
Just pick up the phone to speak with someone who knows what you’re going through, and we’ll help you figure out the rest. You’ll be here and ready to find lasting freedom through sobriety in just a few simple steps.
Stop trying to fight this battle alone. Let today be the day you take control back from addiction. Contact Crest View today.